TMS for Depression: How It Helps
iMind Mental Health Solutions Resource

There is no doubt that depression can be serious. Without treatment, it can become debilitating. At its worst, it can cause suicidal thoughts. About 60 percent – or 420,000 of the over 700,000 people who die by suicide each year – have a mood disorder such as depression.

Depression is not something someone can “snap out of”. It is rooted in brain differences arising from genetics, experiences, and other factors beyond an individual’s control.
That’s why Transcranial Magnetic Stimulation (TMS) holds so much promise for depression: It works directly on the areas of the brain responsible for mood regulation. Dysfunction in these areas can cause depression, and TMS aims to correct it.
With an estimated 30 to 60 percent of people with depression not responding to front-line medication treatment, it is vital to find other options.
Depression Epidemic
Depression is “common” worldwide, with just under four percent of the global population affected. However these rates are much higher in the United States. In fact, the U.S. has the second highest rate of depression on Earth – tied with Australia and just behind war-torn Ukraine – according to World Population Review 2023.
The National Institutes of Health tells us that 8.4 percent of U.S. adults had at least one episode of major depression. In women, rates are yet higher – 10.5 percent, versus 6.2 percent of men. It also impacts younger adults more, with 17 percent of 18-to-25-year-olds having experienced major depression.
“Depression is extremely common in the U.S. and has reached epidemic levels.”
RENEE GOODWIN
Renee Goodwin, epidemiology and biostatistics professor at City University of New York’s Graduate School of Public Health and Health Policy, told U.S. News & World Report that “depression is extremely common in the U.S. and has reached epidemic levels.”
Goodwin feels there are multiple reasons for this, citing “economic distress” and increasing “feelings of helplessness” as two potential ones. Unfortunately, relapse rates for depression are the highest among any medical condition as well.
What is Depression?
Depression is not a passing feeling of sadness. Whether it’s losing a job, breaking up with someone, sustaining an injury, or experiencing a financial setback, all of us can feel depressed at times in response to the trials of everyday life.
Clinical depression, however, is chronic or recurrent and moderate-to-severe in intensity. In fact, people with depression can find it hard to function. They can have trouble getting out of bed, performing their duties at work, and maintaining relationships.
Am I Depressed?
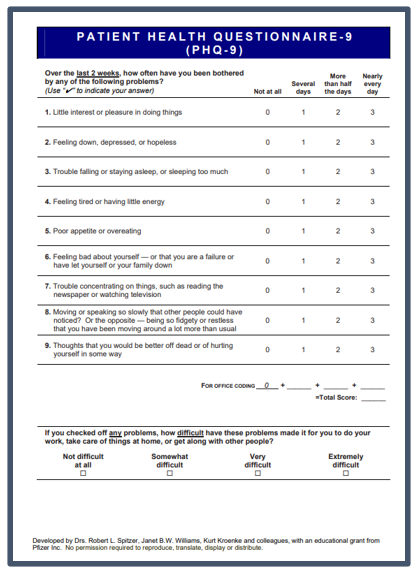
Mental health professionals can use the Patient Health Questionairre-9 (PHQ-9) to gauge the severity of depression. Patients answer the questions themselves, rating symptom intensity on a scale from one to five. These answers are added together to determine an overall score.
What is the PHQ-9 Rating Scale?
0-4 points – Minimal Depression
5-9 points – Mild Depression
10–14 points – Moderate Depression
15-19 points – Moderately Severe Depression
20+ points – Severe Depression
RELATED: Am I Depressed? Take the PHQ-9 Test
The Depressed Brain vs. Normal Brain
Mental illness can be misunderstood. It is not a personal choice. It cannot be readily controlled. It is not unique to an individual; in fact, all of us can be vulnerable to a mental illness at some point in life’s journey.
Mental illness arises from differences in the structure or function of the brain. These differences can be genetic, or they can happen in response to an environmental trigger.
Although the pathophysiology is not completely understood, real, identifiable brain differences have been noted in people with depression.
Dorsal Lateral Prefrontal Cortex (DLPFC) and Depression

Just behind the forehead lies the brain’s prefrontal cortex, or PFC. It is the last part of the brain to develop, reaching maturity at some point in the mid-to-late 20s.
It is responsible for executive functions, or functions that involve controlling impulses and replacing them with goal-directed behavior.
There are several parts to the PFC. One of them – the dorsolateral prefrontal cortex (DLPFC) – plays a key role in mood regulation has been particularly associated with depression.
The DLPFC has been linked with:
Finally, developing and maintaining your connections with other people can create a buffer against stress as well. Don’t neglect getting together with friends or making new ones, as they are good for your mental health.
Studies have repeatedly shown abnormalities in the DLPFC of people with depression, in particular:
- Decreased activity in the left DLPFC and connection to the anterior cingulate cortex, the amygdala and the insula, areas associated with mood regulation. This has been found to be correlated with “negative emotional judgment”.
- Hyperactivity in the right DLPFC, which is associated with severity of depression symptoms and to “attentional modulation”, or controlling what you pay attention to versus what you do not.
Even minor damage to the DLPFC can have an effect. Damage to the DLPFC can manifest as:
- Apathy
- Attention Problems (inattention, problems resolving conflicting stimuli, et al.)
- Blunted Emotional Responses
- Decreases in Goal-Directed Behavior
- Emotional Instability
- Inability to Act Decisively
- Inability to Detect Errors
- Increase in Compulsions
- Indifference to Hunger, Thirst and/or Pain
- Lack of Motivation
- Lack of Spontaneity in Behavior and Language
- Repetitive, Compulsive Behaviors
Many of the symptoms above mirror those with depression, including an overriding sense that “nothing is worth doing” and a lack of interest and engagement with the world.
Neurotransmitters and Depression
Neurotransmitters are the chemical messengers of the brain. They are released by nerve cells, called neurons. Their job is to stimulate neighboring neurons, muscle cells, or gland cells. This allows impulses to be passed from one cell to the next, throughout the entire nervous system.
Three main neurotransmitters are involved in regulation of mood, sleep, appetite, and other functions impacted by depression. There are norepinephrine, serotonin, and dopamine.
Dopamine
Dopamine functions as both a neurotransmitter and a hormone. It is involved in:
- Arousal
- Attention
- Behavior
- Cognition
- Lactation
- Learning
- Memory
- Mood Regulation
- Movement
- Pleasurable Reward
- Sleep
If dopamine levels are low, a person may feel tired, unmotivated, and unhappy. Patients with low dopamine can also experience memory loss, mood swings, sleep problems, trouble concentrating, and a low sex drive.
Norepinephrine
Norepinephrine also functions as both a hormone and a neurotransmitter and impacts:
- Alertness
- Arousal
- Attention
- Impulsive Behavior Control
- Memory
- Mood Regulation
- Sleep/Wake Cycles
Low levels of norepinephrine can cause a variety of health problems, chief among them anxiety and depression.
Serotonin
Serotonin also acts as a hormone and a neurotransmitter and helps:
- Impulsive Behavior Control
- Mood Regulation
- Sleep Quality
Low serotonin levels are associated with decreased energy levels, sadness, feelings of hopelessness and mood swings. Sustained low serotonin levels can lead to anxiety, worsening depression, and even suicidal thoughts.
If levels of these vital chemicals are chronically low, the deficit can also affect other areas of the brain with connections to the DLPFC, such as the insula, anterior cingulate, and the amygdala.
The Insula
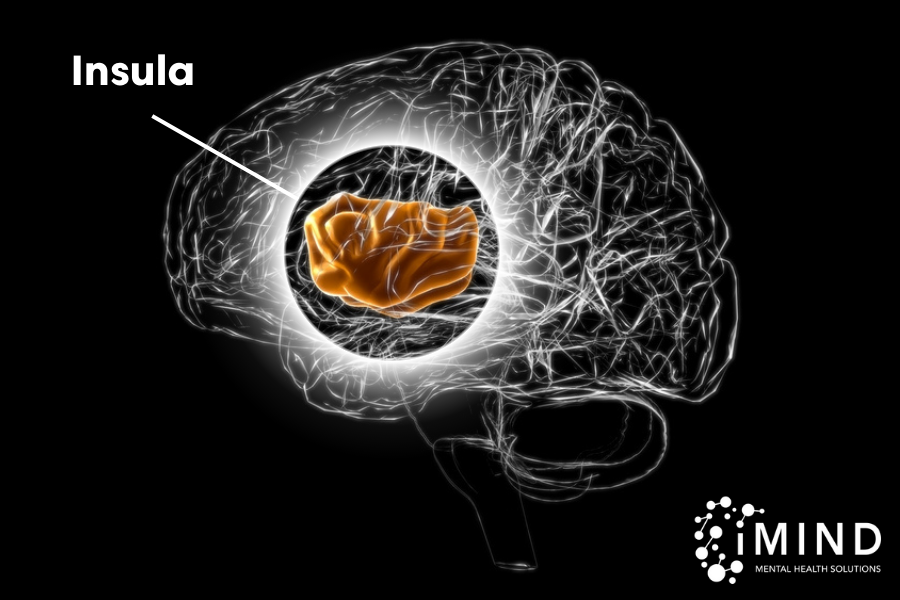
The insula is the part of the brain where the mind meets the body. It is always taking the temperature of your life, and its goal is to keep you in a state of balance, or homeostasis. It’s not letting you get too hungry, too thirsty, too hot, or too cold.
In a 2007 article for The New York Times, Sandra Blakeslee explains the insula’s complex set of functions this way:
“The insula itself is a sort of receiving zone that reads the physiological state of the entire body and then generates subjective feelings that can bring about actions, like eating, that keep the body in a state of internal balance.”
Information gathered from all senses – except touch and spatial awareness – is routed to the insula. Along the way, input is added from the heart, lungs, gut, and other organs. The insula transforms this input into an emotion that prompts a decision.
When you feel hunger, your insula prompts you to eat. You feel thirsty, it goads you to reach for the water bottle. You smell bad food, your nose wrinkles and you feel disgust, thanks to the insula. It even anticipates future events, such as gearing up for cold weather with a physiological response.
“The insula itself is a sort of receiving zone that reads the physiological state of the entire body and then generates subjective feelings that can bring about actions like eating, that keep the body in a state of internal balance.”
SANDRA BLAKESLEE
Studies have found a link between Major Depressive Disorder and abnormalities of the insula, including:
- Decreased activity in the insula when attuning to internal states. Subjects in one study were shown the words “heart,” “stomach,” or “bladder” in order to turn their attention to those areas of the body. In those with depression, insula activity dropped compared to healthy controls.
- Increased connectivity between the insula and the limbic system in a resting state – and this is associated with the severity of depression symptoms. The more “functional connectivity” there is, the more severe the symptoms are.
- A greater volume of grey matter, which correlates with higher scores on depression scales
- Decreased functional connectivity between the DLPFC and the insula, which is associated with more severe depression scores.
MDD and its physical symptoms – such as lack of energy, pains and aches, trouble sleeping or oversleeping, and over or under eating – are associated with abnormal recognition of how the body feels – call interoception, for which the insula is responsible.
One study revealed that, in depression, the processing of emotions was shifted to the same region where pain is processed, possibly accounting for the feeling of emotional pain that people with depression experience.
Further supporting this link is a study of Parkinson’s patients published in 2020 which found that severely damaged insula networks in these patients contributed to depression. A damaged insula can also cause a loss of libido, the ability to discern whether a food is fresh or spoiled, and apathy.
The Anterior Cingulate Cortex & Depression
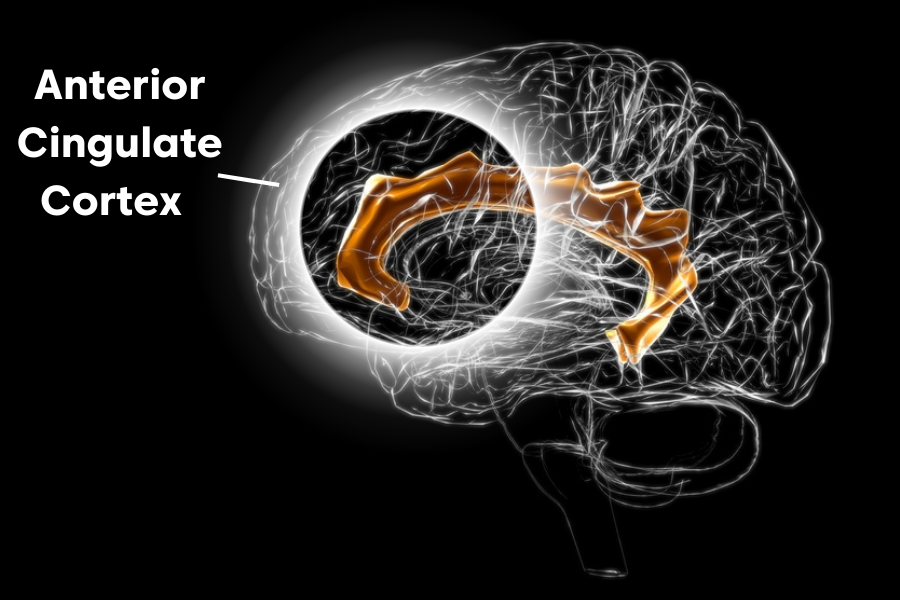
With connections to the thinking brain (prefrontal cortex) and the feeing brain (limbic system), the anterior cingulate cortex acts as a go-between to the two regions. It is responsible for higher-level functions such as:
- Anticipating a Reward
- Allocating Attention
- Autonomic Nervous System Response
- Controlling Impulses
- Detecting Error
- Emotional Awareness & Expression
- Ethics and Morality
- Impulse Control
- Making Decisions
- Managing Pain
- Monitoring Performance
It is especially critical for controlling and managing our emotions, which is an important part of treating depression. Problems with the anterior cingulate cortex (ACC) are associated with feeling depressed as well as persistent feelings of sadness.
There are two main regions to the ACC: the pregenual (pACC) and subgenual or subcallosal (sACC) regions. Brain differences in the latter have been found in those with MDD versus those without. In particular:
- The subgenual ACC is smaller in people with depression; however, activity is proportionately greater, given its size. This increased activity can be found when people experience sadness in a “baseline resting state” – and the more activity there is, the greater degree of sadness is felt. What’s more, hyperactivity here can predict whether someone will experience treatment-resistant depression.
- There is less functional connectivity between the two parts of the ACC (pACC and sgACC), which can be the reason that negative emotions persist with depression.
In simple terms: If you find it hard to break out of negative emotions and are constantly ruminating on the negative (“bad things always happen to me”, etc.) that’s happening in the ACC.
The Amygdala & Depression
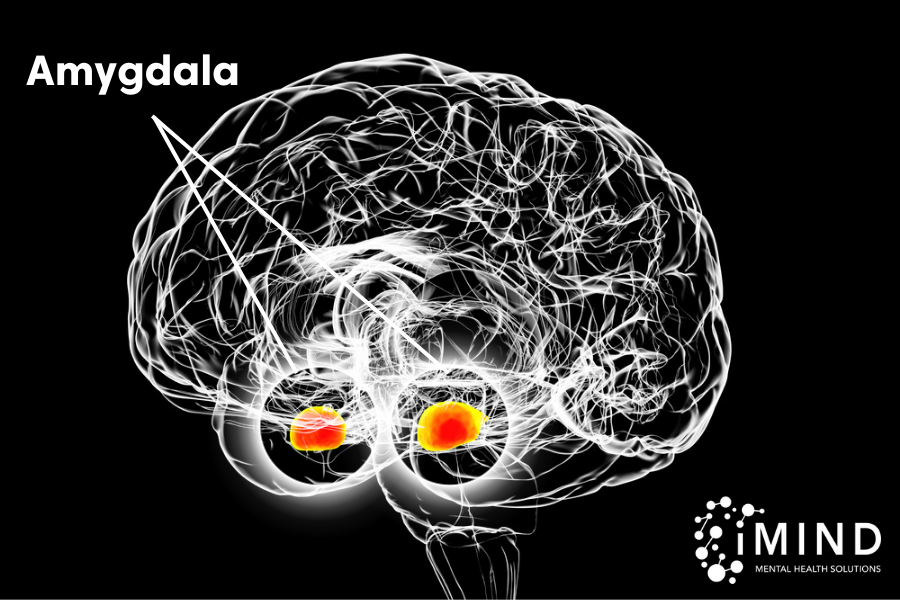
Two almond-shaped organs collectively called the amygdala are nestled on either side of the brain. They act as our emotional center, playing a role in:
- Emotion Generation & Response
- Perception of Emotions
- Interpreting What is Going on Around us
- Autonomic Responses
- Directing Attention
- Emotional Memory Formation
- Fear Conditioning
In short, the amygdala is responsible for how we feel about the situations and events of our lives. It is also always on the lookout for potential threats, continuously scanning our surroundings for them, then sending messages to the PFC and ACC that trigger an immediate emotional response. You aren’t sure why you are feeling fearful or panicked, but you picked up something in the environment – such as an angry facial expression – that triggered the amygdala’s fight-or-flight response.
In people with depression:
- The amygdala is larger and overactive. This can lead to overwhelming negative emotions, a hard time “shutting your brain off” to rest, and an inability to cope with the stress of everyday life. Because the amygdala is more oriented to negative stimuli, overactivity here can lead to a negative bias, or a tendency to view the world in a not-so-favorable light.
- There is decreased connectivity of the amygdala to other areas of the brain controlling emotions. This further enforces the experience of overwhelming emotional states as well as “impaired social cognition,” or the ability to properly interpret and store information about people around us, as well as an outsized response to negative cues.
How TMS Works for Depression
The connections between a disruption in neurotransmitter production and its effects on multiple areas of the brain with depression are obvious. These chemicals are vital for a healthy brain and good mental health.
Many anti-depressants on the market aim to increase levels of one or more of these neurotransmitters. For those with treatment-resistant depression, however, those medications fail to make a real difference in symptoms.
That’s where TMS comes in. TMS helps correct the symptoms of depression by stimulating the areas of the brain that produce these chemicals.
TMS Targets the DLPFC and Its Network
TMS works by targeting the DLPFC, which is underactive in depression and very close to the surface of the scalp. It responds to the magnetic stimulation of the TMS machine, and its connectivity to other regions allows TMS treatment to effectively reach those other structures as well.
TMS magnetic coils generate magnetic fields similar to those produced by MRI (magnetic resource imaging) equipment. However, the TMS field is much smaller and more concentrated, targeting an area just two to three centimeters in size.
The brain responds to this stimulation by generating small electric currents that encourage neurotransmitter production – including the same ones lacking in those with depression… dopamine, norepinephrine, and serotonin.
TMS Retrains the Brain
Over the course of treatment, TMS causes the brain to form new neural pathways. Neurotransmitter levels return to normal and, over time, the brain is “trained” to stay in this state.
Patients begin to experience better moods, lessened anxiety, more pleasurable feelings, and feel more motived. Energy levels are boosted and physical symptoms such as aches and pains are alleviated.
It’s not that you will never need TMS again, but, unlike medication, its effects do last longer than treatment duration. In fact, more than a year of symptom relief is the typical response.
TMS Success Stories
It’s always helpful to hear first-hand accounts about a promising treatment. Over the 15 years that TMS has been used for depression, many success stories have accumulated. Here are but a few:
Marsha Terry suffered from depression for most of her life and had tried five different anti-depression medications without success. She had this to tell CBS Mornings about the relief she experienced with TMS:
“I would say after the first week, I was for sure sleeping better. It’s weird, I started noticing things around me more. One thing recently that happened, about a week ago, we were walking home, and out of the blue, it popped into my head, and I said, ‘I love life.’ I’ve never said that in my life before.”
Terry says she will definitely seek repeat TMS treatment in the future, should her depression symptoms ever return, and adds, I will never give up again, and I have so much hope.”
– Marsha Terry.
Benjamin, a 26-year-old chef in Seattle, told Men’s Health Magazine in 2018:
It really took a lot of my closest friends and family to start noticing these differences. I talk with my dad, and he’s like, ‘Your demeanor has changed. You just sound happier.’
My best friend at work, she’s like, ‘Yeah, you just look better – even as far as your posture goes, just the way you carry yourself.”
I’m feeling like myself again.
After these treatments, I feel like I’m more connected with myself and the world around me, and I can truly say that I’m happy with myself. I like me. It took a long time to get to that point, but throughout depression, I kind of hated myself. I hated life, I hated who I was. Now I have a lot more clarity – I’m even thinking about my future.
Interestingly enough, I’ve been entertaining the idea of going into the mental health field. I don’t know exactly what I’d do, but I just like the idea of helping people with depression or other mental illnesses. I want to give people the hope that I was given – to tell people it’s okay, this isn’t a forever thing. You can overcome this.”
– Benjamin.
Kevin D., a native of Louisiana now living in Port St. Lucie, said of his 2021 TMS treatment at iMind Mental Health Solutions:
“I’ve struggled with anxiety and depression for the better part of my adult life. I turned to medications and different self-help remedies throughout my struggle. Although some medications had some resolution, the side effects always outweighed the relief. I’ve never been a fan of medications, just because of the way it made me feel. Getting off them was also a challenge after developing somewhat of a dependency.
When I was introduced to TMS, I was skeptical yet intrigued. After the first week of my treatment, I began to notice how well my sleep patterns have changed. Getting a good night’s sleep was a small yet pleasant victory.
As I entered my third week of TMS, I felt like a fog had been lifted completely. Things were looking up and my perception of my personal problems did not hold the same weight it used to.
I became more focused on my work, keeping my home and personal spaces clean, and even began to start exercising again. My relationship with my young daughter improved due to the fact that I’ve become way more tolerant. Although I hate to admit it, at times I had a short fuse with her, and in return would feel guilty and embarrassed after a “blow up”. Those type of outbursts have significantly subsided.
I’m truly grateful I took the suggestion and started TMS. It’s genuinely improved all aspects of my life. Today I look forward to waking up and tacking each day the best I can. Even when I’m not as productive as I want to be, I’m not hard or negative on myself anymore. I can confidently say that my depression and anxiety have significantly subsided and would argue that they are gone altogether.
[TMS is] allowing me to be the best version of myself!”
– Kevin D.
Michelle was treated at a Massachusetts practice. She had tried several antidepressants before turning to TMS, which made all the difference for her.
“What depression is like… The best thing I can think of now to describe it is that you’re carrying a 50-pound weight, but you can’t ever put it down. As soon as you get out of bed, you put this weight on and you carry it all day.
It takes so much energy for me to get out of bed in the morning, a monumental effort to do that. And I think people probably think you’re exaggerating, and like, ‘How could it possibly be like that?’ But it is.
It was difficult… We would try medication for a little, (and) it would help for a little, (but) then I would have side effects that would be as bad and would require medication to counter those.
After a couple of weeks (of TMS treatment), I had to fill out a piece of paper to say how I was doing. And I noticed that instead of having things that were not well being all the time, or almost all the time… it started to move. That told me that I have really experienced something dramatic. It changed my whole life.”
– Michelle.
Sam Peterson, a U.S. Army veteran who was a bomb disposal technician and went to Afghanistan, and suffers from depression, as well as anxiety and PTSD, said TMS is helping him to turn the corner. After 35 TMS treatments, he had this to say:
“I felt a pretty significant difference, especially with the depressive symptoms. Stressors are easier to deal with and my lows don’t feel as low.”
– Sam Peterson.
This is but a handful of the many TMS success stories that are out there. The important thing to remember, though, is that research backs up the good results.
What the Research Says About TMS
These benefits of TMS treatment have been confirmed by many clinical studies. Most promising among them is a recent study of 103 TMS providers treating over 5,000 participants. Researchers found that up to 82 percent responded to treatment, meaning that participants experienced improvement in depression symptoms. This is in line with the typically quoted success rate on TMS provider websites, which fall in the 70 to 80 percent range.
What’s more, in the study, up to 62 percent of those 5,000 people experienced total remission. This means that their depression symptoms resolved completely.
“Superior” clinical outcomes tended to be achieved in women and those who received more treatment pulses per session.
Post-Partum Depression
TMS works for post-partum depression as well. One study found that nearly 82 percent of those receiving TMS treatment responded to it, versus 46 percent of the group receiving sham (the procedure equivalent of a placebo) treatment.
Another study found eight out of nine sufferers experienced remission from post-partum depression with repetitive TMS (rTMS). Seven of the nine also stayed in remission, without the use of medications.
TMS is FDA-Cleared & Covered by Insurance
TMS has been cleared by the US Food and Drug Administration for use in major depressive disorder and covered by a wide range of insurance providers.
Both private carriers such as Blue Cross Blue Shield and as well as government plans, including Medicare Part B and Tricare, cover TMS sessions, subject to deductibles and copays.
Patients must meet the criteria, of course. Typically, they must have tried at least two antidepressants without success. An estimated one-third to one-half or more of people with Major Depressive Disorder fit into this category.
Why Should We Care About TMS for Depression?
Depression is one of the leading causes of disability worldwide. It has been described as a black cloud, a heavy weight, and a feeling of separation from others. It can cause severe impairment in an individual’s life, as well as affecting those surrounding them, and increase the risk of suicide.
Depression Affects All the Lives it Touches
It’s not just the person who has depression who suffers. Their loved ones, their children, their friends, their employers and their co-workers are affected by it as well. People with depression also tend to earn less on the job, which affects those who are dependent upon them.
As if that weren’t enough, the economic cost of depression was estimated at a staggering $236 billion five years ago – a 35 percent increase over 2010 estimates. This includes:
- Direct costs of treatment, from counseling to medication and ER admissions
- Costs to employers, including missed workdays and reduced productivity
- The cost of suicide
This does not include raised prices from businesses to make up for their losses due to depression. For every dollar spent on direct treatment, it costs all of us another $2.30 on indirect expenses.
Without a doubt, though, it’s the high human cost of depression through debilitation and suicide that is truly devastating.
Hope for Treatment-Resistant Depression
If I can stay in bed all day, that’s what I do… I just want to be able to live my life.”
RINI KRAMER CARTER, IN AN INTERVIEW WITH PBS
Rini Kramer-Carter told PBS her treatment-resistant depression severely affects her life, causing her to sleep as much as 20 hours a day. “If I can stay in bed all day, that’s what I do… I just want to be able to live my life.”
Unfortunately, she is not alone. Up to 60 percent of people with depression do not adequately respond to first-line treatments of therapy and medication.
Treatment resistant depression can be challenging, as patients have already experienced:
- A lack of response to treatment
- After a minimum of two trials of two different anti-depressant medications
- For a minimum of four to six weeks each
Due to an ongoing nationwide shortage of psychiatrists in the United States, most people are seen by primary care doctors, who are overwhelmed with patients already. Over 50 percent of the counties in the U.S. do not even have one psychiatrist.
“Given a shortage of geriatric psychiatrists, decisions on treatment are often left to primary care providers, who may not have relevant training or might be reluctant to take on such complicated care,” said Evelyn Whitlock, Patient-Centered Outcomes Research Institute’s Chief Science Officer, said. “They try something, and, if it doesn’t work, they try something else… trial and error is not ideal”
There is a compelling need for new treatments to counteract treatment-resistant depression, and TMS fits that bill. It is clinically proven effective, safe, and FDA cleared to tackle this hard-to-treat condition.
While locally sponsored efforts are now underway to educate primary care providers and their patients about TMS, it remains a treatment promise that, much more often than not, delivers real results to depression sufferers who need it most.
About the Author

Justin Baksh
LHMC, BC-TMH, Chief Executive Officer
Justin’s desire to help others struggling with mental health issues led him to pursue a career in counseling after completing his service in the United States Marine Corps. Today, he has over a decade of successful experience as a counselor, both in private practice and as the CEO at iMind Mental Health Solutions. His experience working with a wide variety of mental health conditions has developed his empathetic, down-to-earth style. His expertise has been called upon for numerous speaking engagements and he is frequently quoted in the media, including prestigious sites such as Buzzfeed, Huffington Post, Bustle, Rewire, and Healthline. Justin holds a Master’s in Mental Health Counseling and is a licensed mental health counselor as well as a Board Certified TeleMental Health Provider (BC-TMH).
- Avery, J. A., Drevets, W. C., Moseman, S. E., Bodurka, J., Barcalow, J. C., & Simmons, W. K. (2014). Major Depressive Disorder Is Associated With Abnormal Interoceptive Activity and Functional Connectivity in the Insula. Biological Psychiatry, 76(3), 258–266.
- Blakeslee, S. (2007, February 6). A Small Part of the Brain, and Its Profound Effects. The New York Times.
- De Risio, L., Borgi, M., Pettorruso, M., Miuli, A., Ottomana, A. M., Sociali, A., Martinotti, G., Nicolò, G., Macrì, S., di Giannantonio, M., & Zoratto, F. (2020). Recovering from depression with repetitive transcranial magnetic stimulation (rTMS): a systematic review and meta-analysis of preclinical studies. Translational Psychiatry, 10(1), 1–19.
- Ettman, C. K., Cohen, G. H., & Galea, S. (2020). Is wealth associated with depressive symptoms in the United States? Annals of Epidemiology, 43, 25-31.e1.
- Filatova, E. V., Shadrina, M. I., & Slominsky, P. A. (2021). Major Depression: One Brain, One Disease, One Set of Intertwined Processes. Cells, 10(6), 1283.
- Garcia, K. S., Flynn, P., Pierce, K. J., & Caudle, M. (2010). Repetitive transcranial magnetic stimulation treats postpartum depression. Brain Stimulation, 3(1), 36–41.
- Grimm, S., Beck, J., Schuepbach, D., Hell, D., Boesiger, P., Bermpohl, F., Niehaus, L., Boeker, H., & Northoff, G. (2008). Imbalance between Left and Right Dorsolateral Prefrontal Cortex in Major Depression Is Linked to Negative Emotional Judgment: An fMRI Study in Severe Major Depressive Disorder. Biological Psychiatry, 63(4), 369–376.
- Health (US), N. I. of, & Study, B. S. C. (2007). Information about Mental Illness and the Brain. In National Institutes of Health (US).
- How deep transcranial magnetic stimulation changed one woman’s life. (n.d.). https://youtube.com. Retrieved April 4, 2023,
- Huang, P., Guan, X., Guo, T., Zeng, Q., Xuan, M., Gu, Q., Xu, X., Zhou, C., Wu, J., & Zhang, M. (2020). Damaged Insula Network Contributes to Depression in Parkinson’s Disease. Frontiers in Psychiatry, 11, 119.
- Ibrahim, H. M., Kulikova, A., Ly, H., Rush, A. J., & Sherwood Brown, E. (2022). Anterior cingulate cortex in individuals with depressive symptoms: A structural MRI study. Psychiatry Research: Neuroimaging, 319, 111420.
- Kandilarova, S., Stoyanov, D., Kostianev, S., & Specht, K. (2018). Altered Resting State Effective Connectivity of Anterior Insula in Depression. Frontiers in Psychiatry. 9.
- National Institute of Mental Health. (2022, January). Major Depression. National Institute of Mental Health.
- Psychiatry.org – The Economic Cost of Depression is Increasing; Direct Costs are Only a Small Part. (2021, May 27). Psychiatry.org.
- Rudebeck, P. H., Putnam, P. T., Daniels, T. E., Yang, T., Mitz, A. R., Rhodes, S. E. V., & Murray, E. A. (2014). A role for primate subgenual cingulate cortex in sustaining autonomic arousal. Proceedings of the National Academy of Sciences, 111(14), 5391–5396.
- Sackeim, H. A., Aaronson, S. T., Carpenter, L. L., Hutton, T. M., Mina, M., Pages, K., Verdoliva, S., & West, W. S. (2020). Clinical outcomes in a large registry of patients with major depressive disorder treated with Transcranial Magnetic Stimulation. Journal of Affective Disorders, 277, 65–74.
- Schwartz, J., Ordaz, S. J., Kircanski, K., Ho, T. C., Davis, E. G., Camacho, M. C., & Gotlib, I. H. (2019). Resting-state functional connectivity and inflexibility of daily emotions in major depression. Journal of Affective Disorders, 249, 26–34.
- Sliz, D., & Hayley, S. (2012). Major Depressive Disorder and Alterations in Insular Cortical Activity: A Review of Current Functional Magnetic Imaging Research. Frontiers in Human Neuroscience, 6.
- Somani, A., & Kar, S. K. (2019). Efficacy of repetitive transcranial magnetic stimulation in treatment-resistant depression: the evidence thus far. General Psychiatry, 32(4), e100074.
- Stevens, F. L., Hurley, R. A., & Taber, K. H. (2011). Anterior Cingulate Cortex: Unique Role in Cognition and Emotion. The Journal of Neuropsychiatry and Clinical Neurosciences, 23(2), 121–125.
- The Amygdala: Definition, Role & Function – Video & Lesson Transcript | Study.com. (2015). Study.com.
- The Drugs Didn’t Work. So I Tried to Cure My Depression With Brain Magnets. (2018, May 24). Men’s Health.
- The Editors of Encyclopedia Britannica. (2018). neurotransmitter | Definition, Signaling, & Types. In Encyclopædia Britannica.
- TMS helps some patients with anxiety and depression. (2022, July 26). FOX31 Denver. https://kdvr.com/news/local/tms-transcranial-magnetic-stimUniversity of Queensland. (2018, July 4). Depression and the brain. Uq.edu.au.
- U.S. Department of Health & Human Services. (2015, August 21). Does depression increase the risk for suicide? HHS.gov.
- What happens when someone has “treatment-resistant depression”? (2016, October 4). PBS NewsHour.
- World Health Organisation. (2021, September 13). Depression. WHO.
Latest News
-
Top 10 Questions About Art Therapy for Mental Health
Art therapy has recently gained recognition for its unique blend of healing therapy and personal expression. Despite its growing popularity, there seems to be some misunderstanding about what art therapy entails, who it can benefit, and how it differs from other forms of therapy.
-
ADHD Strengths: The Positive Side of Attention Deficit Hyperactivity Disorder
Scattered minds, fidgety bodies, and difficulty focusing. Attention Deficit Hyperactivity Disorder (ADHD) often gets painted in shades of struggle. But what if there’s a brighter side to the story? What if, beneath the challenges of ADHD, lie unique strengths just waiting to be unlocked?
-
Sunshine and Smiles: Does Living in a Warm Climate Guarantee Happiness?
While the allure of tropical paradises might seem straightforward, the relationship between climate and happiness is far more nuanced. Grab your metaphorical mug of hot coffee (or iced, depending on your climate!), and let’s embark on a journey to understand: Are people in warmer climates truly happier, or is this just another sun-kissed illusion?



